VikingsGuy
Well-known member
HT has threads to discuss covid-19 effects on wall street, covid-19 humor, covid-19 effect on hunting seasons, but thought some may appreciate aggregating links (and thoughtful discussion) regarding emerging understanding of treatment/vaccine options. Let's listen and learn from one another. Disagreement is fine, but should be based on scientific critique or counter-posts, not memes, politics, generalized attacks on the pharma industry or conspiracy theory.
He is a recent article I offer for your reading:

 www.wsj.com
www.wsj.com
He is a recent article I offer for your reading:
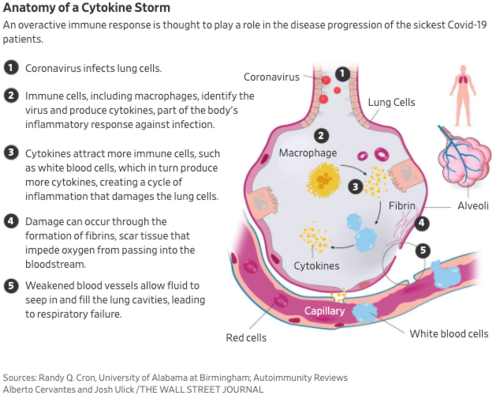
Haywire Immune Response Eyed in Coronavirus Deaths, Treatment
An immune system gone haywire may be doing more damage than the coronavirus itself in patients with the severest forms of Covid-19, doctors and scientists say, a growing theory that could point the way to potential treatments.